What is Melasma? Stable Vs. Unstable, Causes and Treatment
The dark patches of Melasma are the result of excessive melanin being produced by melanocyte cells in the skin.
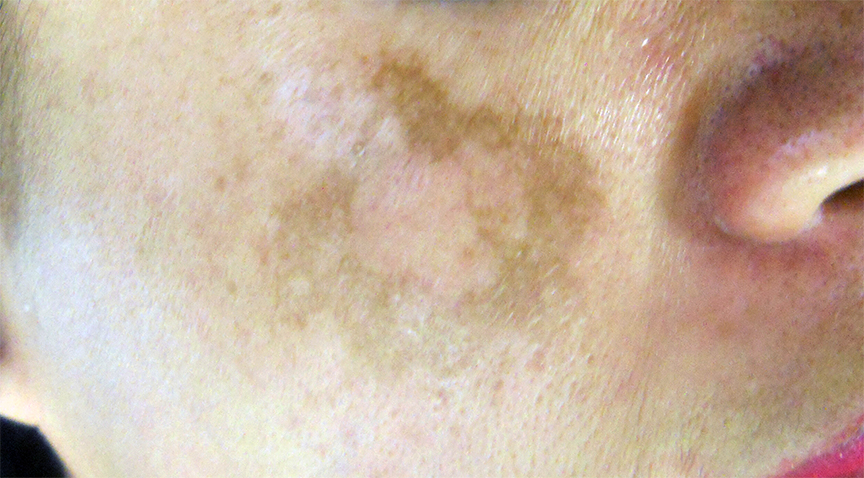
Melasma is a very difficult and tricky skin condition to resolve. It appears as dark patches of pigmentation on the skin that often sneaks up onto a woman’s face. One day out-of-the-blue, she suddenly notices a dark shadow or “patch” appearing on her face.
The hyperpigmentation can vary from wide and diffuse to a bunch of smaller dark spots (like freckles) that never bothered her before, that suddenly grow bigger and darker and merge into a single larger dark patch on her face.
A Ride on the Melasma Merry-Go-Round

The dark patches of melasma on the cheek.
This sudden realization that something is happening to her skin’s pigmentation is often accompanied by friends who say things like: “hey what happened to your skin?” They may even target your face with a damp cloth and say: “hang on a minute… let me help you with that stuff on your face”.
Typically, this Oh-My-God! moment is quickly followed by the sound of screeching tires as you fish-tail out of the driveway on your way to the mall in search of a magic potion that will fix your discolored skin.
Fancy Products and Treatments Can Make the Melasma Worse
Unfortunately, if the evil dark patches of hyperpigmentation invading your skin are a melasma, you will likely end up throwing away hundreds of dollars (if not thousands) on fancy products hyped up with fanciful promises that produce little to no results. In fact, if you throw too many products at your already unhappy skin you may cause even more irritation, which might make the dark patches of hyperpigmentation even worse.
Disappointment with products is quickly followed by frustration with skin spas, countless facials, all sorts of peels, and maybe even a series of dermatologists who pronounce that nothing can be done, leaving you depressed and hopeless.
Usually, melasma is an ill-fated story dominated by a downwards spiral of negative results, increasing amounts of wasted hard-earned-dollars, bitter frustration and emotional anguish.
Because it’s easy to make your hyperpigmentation worse, and waste a lot of money chasing your tail on the melasma merry-go-round, it’s important to understand what is happening in your physiology; what treatments for melasma are likely to work or not work; and what treatment strategy produces the best results and why. Finally, when a solution appears that can work for you, it’s not an accident that it does, and your understanding of your own skin will play an important role in a successful outcome.
What is Melasma?

An overproduction of melanin is what causes the dark patches of skin.
Melasma (muh-LAZ-muh) is a skin disorder that is most prevalent in women of medium and darker skin tones though it can affect women of all skin tones, especially if her genetic heritage contains even a small compliment from darker ethnicities.
The dark patches of hyperpigmentation are caused by excessive melanin being produced on the sun-exposed areas of the skin. Melasma is most likely to appear in women experiencing hormonal fluctuations caused by pregnancy, while taking contraceptive pills or hormone replacement therapy. The risk is even higher in those who are over-exposed to sunlight or who have endured chronic irritation from external factors such as chemicals, abrasions, and even waxing.
Usually, melasma first resembles the appearance of sunspots and later progresses into a more “mask-like” uneven, patchy and brown-toned discoloration. Hence the term: “the mask of pregnancy”. These dark patches can appear on the cheeks, nose, lips, and/or forehead.
The 3 Patterns of Melasma
Melasma appears in three distinct patterns on the face.
- Centro-Facial: is identified by dark patches on the center of the face. This is the most common occurrence as it appears on the upper lip, chin, forehead, cheeks and nose.
- Malar Pattern: is identified by dark patches on the upper cheeks.
- Mandibular Pattern: is identified by dark patches on the jaw.
While not as common, melasma may also be found on other parts of the body including the upper sides of the neck and the forearms (Extra‐facial melasma).
The 4 Types of Melasma
Melasma is almost always diagnosed during a visual skin exam by dermatologists or skincare specialists. Unfortunately, most cases are diagnosed after the onset of the dark patches of skin. A Wood lamp or black light can help doctors identify melasma in the early stages if you are suspicious.
-
What the dark patches of skin look like under a UV light.
Epidermal Melasma: This type occurs when extra melanin is found in the exterior layers of the skin (epidermis).
- Dermal Melasma: This type is when melanin-digesting cells, called melanophages, are discovered in various layers of the skin (dermis).
- Mixed Melasma: This type is a combination of the epidermal and dermal types.
- Finally, the fourth type does not have a name but is characterized by melanocytes in dark-skinned patients. In rare cases, skincare specialists may need to perform a skin biopsy for diagnosis.
Luckily, the dark patches of skin will naturally fade in most cases. The fading is particularly common when the cause of the melasma is a change in hormones, such as pregnancy. However, in some cases, the dark patches will not fade and can last for years.
What Causes Melasma?
Nobody really knows exactly what causes melasma. Here are the possibilities:
Watch the video : Melasma, A Deep Dive into the Cause & Treatment
1. Hormones

Melasma can be caused by a fluctuation in hormones.
There is a definite correlation between hormonal fluctuations and melasma, such as during pregnancy when the dreaded “mask of pregnancy” appears. Furthermore, the skin of some women is so sensitive to hormonal fluctuations that going on birth-control medication, stopping birth-control medication or even changing brands of birth-control medication can provoke a melasma. Bottom line, in some women of mid-color skin, melanocytes are sensitive to hormones.
- But why then do only some areas of the face get darker and not others?
- Why not the entire face, or any other sun exposed skin on the body?
- Why are many women who are not experiencing any measurable hormonal fluctuations still plagued with it?
Once again, nobody really knows.
2. Irritation to Skin – Post Inflammatory Hyperpigmentation (PIH)

Post Inflammatory Hyperpigmentation (PIH) is different from melasma.
Irritation to the skin can cause excessive pigmentation in mid-color skin of both men and women. For instance, for women who wax, thread or pluck the hair on their upper lip, after years of this irritation, the traumatized melanocytes become hyperactive and cause localized hyperpigmentation. This is classified as “post inflammatory hyperpigmentation” (PIH) and though it may look like melasma, it technically is not.
Another common example of PIH, is the pigmentation due to cystic acne… especially if you have aggravated the situation by picking at it. Even after the cyst has resolved, the dark PIH spot may linger for weeks, even months, depending on the type of skin you have. Once again, men and women who have mid-color skin… of “unlucky duckling in the middle” are most susceptible to PIH.
What is true however, is that for some, what started as localized PIH may have slowly spread and become what presents as a melasma. It is very important to discern this during the initial consultation.
3. Excessive Sun Exposure

Sun exposure is also believed to be a cause of melasma.
As in B. above, a sun burn is a significant irritation to the skin and over time can provoke a melasma in mid-color skin types of both men and women.
Question: Given all the things we don’t know, can melasma be successfully treated?!
Answer: Yes, it can be successfully treated… but first we must distinguish between a stable and an UN-stable melasma.
Stable Vs. Unstable Melasma
Generally speaking, there are two main categories of Melasma – Stable and Unstable.
Stable Melasma
Simply stated, a stable melasma is one that does not change much from day to day or week to week. It stays pretty much the same. Additionally, it does NOT easily flare up when exposed to a few minutes of sun.

A stable melasma pretty much stays the same from week to week.
To understand this better, imagine a pregnant woman, who during her pregnancy develops a melasma. Obviously, the hormonal fluctuations of pregnancy provoked it. Once her baby is born and her hormones return to normal, the melasma tends to resolve on its own as the over stimulated melanocytes calm down. However, in some cases it persists, but is stable. Simply understood, given that the underlying hormonal fluctuations that caused it have resolved, the melasma is no longer “motivated” to grow or spread. It seems therefore that the melanocytes that were over-producing melanin during the pregnancy are now “stuck” at this higher level of melanin production.
A good analogy is a house with many rooms, each of which has a thermostat set at a perfect temperature of 72 degrees. But then, something happens to the house, and the thermostat of one room is upset and stuck at 80 degrees, and thus, is always hotter than all the other rooms. Essentially, in a stable melasma, the melanocytes in a certain area of the skin are upset and stuck at a higher level of melanin production.
This kind of stable melasma has a very good chance of being successfully treated, as I will describe later in this article on laser treatment for melasma.
Unstable Melasma

An unstable melasma is constantly changing or spreading.
Simply stated, an unstable melasma is constantly shifting, is easily provoked to getting darker, and is extremely sensitive to any sun exposure. Even exposure to heat, on a hot day or a hot-tub can make the it flare up. Simply explained, there is some underlying cause that is making this unfortunate woman’s melanocytes hypersensitive and hyper-reactive.
In an unstable melasma, even when the extra melanin is successfully removed from a woman’s skin, it tends to come back in a matter of weeks, even days… because some mysterious underlying condition is constantly instigating the melanocytes to produce extra melanin.
Melasma Treatment Options
Many dermatologists won’t treat it…
Why?
Because they fear making the melasma worse… resulting in a patient that is even more unhappy than when they first walked through the office door.
Many dermatologists will only go as far as prescribing a hydroquinone “bleaching” cream… which typically will lighten the skin until you stop using it, only to have the melasma come right back.
Watch the video : My experience with laser melasma treatment
Topical Creams

Hydroquinone is applied directly to the skin to lighten it.
Some medications are available to help lighten the dark patches of skin. The most common and best cream for this is Hydroquinone. Hydroquinone comes in a lotion, gel, liquid or cream form and is applied directly onto the skin. Some forms of Hydroquinone can be obtained without a prescription from your doctor. However, they are diluted and prescription medications may give you quicker results.
Tretinoin (Retin-A) and Corticosteroids are often used along with Hydroquinone creams to lighten the dark patches of skin. The two ingredients are often found together in a medication prescribed by your dermatologist or skincare specialist. Some creams may also contain Kojic acid or Azelaic acid.
Microdermabrasion and Chemical Peels
The quickest way to get rid of the dark patches is through procedures such as chemical peels with Glycolic acid. Other hands on treatments include microdermabrasion and dermabrasion. By far the most effective treatments for melasma use lasers.
Once your melasma has cleared your skincare specialist may recommend maintenance therapy to help prevent against future outbreaks. Your skincare provider may recommend applying daily sunscreen, wearing a wide brimmed hat or using oxide or titanium oxide to block the suns rays.
Laser Treatment
No two cases of melasma are the same, each requires an individualized assessment of the hyperpigmentation and a customized laser treatment protocol. In many cases, in order to “consult the patient’s physiology” we will perform a number of small test treatments on a given patient in order to establish which laser protocol their skin responds to best. We do not charge for these test treatments.

Before and after laser melasma treatment.
Lastly, in cases of an unstable melasma that is resisting treatments, we often “go back to the drawing board”, administer additional tests with a variety of laser technologies and protocols, in order to get the skin “back on track”. We also do not charge for these treatments.
Melasma can cause a variation of skin discolorations depending on the concentration, density, and depth of melanin at different locations within the affected area. Thus, the most successful treatments often necessitate an array of different lasers.
We have over 25 lasers, a number of which can be effectively used for dark patches on the skin. Given that we specialize in using lasers in combination, there are a large number of protocols that can be employed to advance progressively better results. We also integrate other holistic modalities with our laser protocols, such as Physiological Regulating Medicine, Hyperbaric Oxygen Therapy, pharmaceutical and natural lotions, and IV Nutritional Therapy.
Please note, that with ALL medical technologies, the magic of producing satisfying results is not inherent in the technology itself, but in how it’s used; in the insight of the practitioner, and the customization of the protocol according to the particular needs of the specific physiology that is being treated.
Watch the video : What is laser melasma treatment?
Bottom line, when a patient’s melasma is not resolving as we all hoped, we go the extra mile – at our own cost – to do whatever we can to get better results. We hope that our patients will be patient with their own skin and with us, as we search for the best customized solution to their individual condition. It truly matters to us.
We truly understand and embrace the frustration that any patient might have with their melasma. We hope that anyone suffering from the dark patches who is reading this, might be willing to give her/his skin and our practice the necessary time to figure out the best course of treatment for his/her particular condition.









